Give Health Plan Members Timely Updates With Texting
Whether it's news about benefits, coverage changes, renewals, or appointment reminders, timely communication is crucial for health plan members. After all, healthcare is a critical service and most people want to act quickly if something changes with their care.
The Short Version
- Members need timely, relevant information from health plans.
- Phone calls and emails can be effective but are not always preferred for timely updates or action items.
- Texting has high reach and open rates. What’s more, SMS offers a convenient way for members to get information and take action.
- Adding texting outreach can improve members’ satisfaction and health outcomes while controlling unneeded healthcare costs.
- Conversational outreach offers AI-powered SMS conversations for even better health plan member engagement.
In today's fast-paced world where instant access to information is the norm, traditional methods like phone calls and direct mail sometimes fall short. Even email doesn’t always offer the immediacy you would expect. About 37% of consumers check their email just once a day or less (HubSpot) and 14.3% of emails aren’t delivered or get caught in spam filters (Emailtooltester).
So how can health plans provide members with the timely updates they need? Let’s explore ways that plans can accommodate their members’ communication preferences, including by using texting. We’ll also discuss the benefits this can have for both the plan and its members.

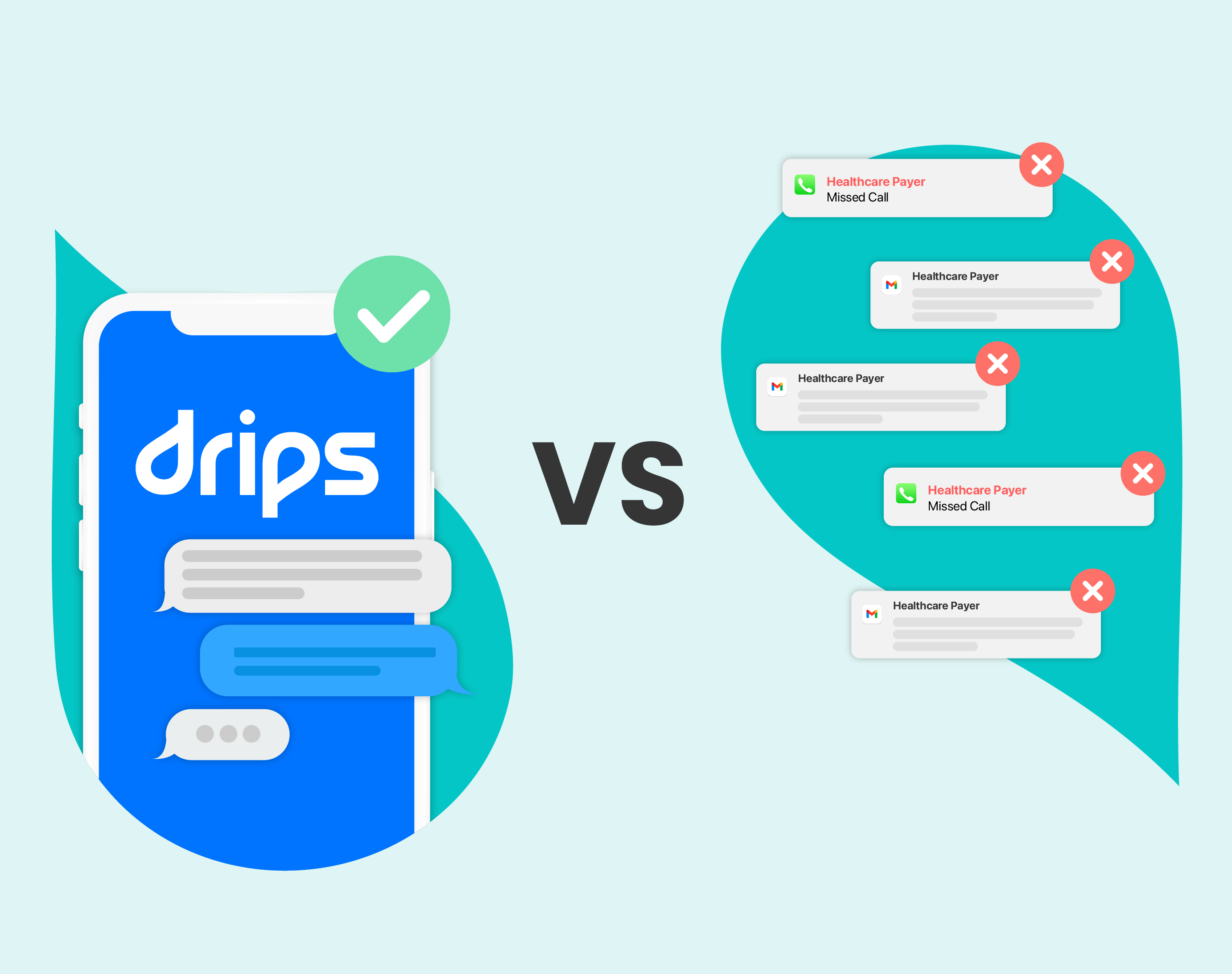
Outbound Dialing Isn’t Always The Best Option
Many health plans currently rely on outbound dialing as a primary method to communicate with their members. This method is familiar for plans and members alike, and it can offer a great chance to connect empathetically with members.
However, phone calls aren’t best for everyone. Many consumers won’t be available to take a call for much of the day. They will likely be working or tied up with other responsibilities. Some health topics are also sensitive, leading people to avoid talking about them in public places.
And that’s if members choose to pick up the phone at all. Eight in 10 Americans don’t answer the phone when the call is from an unknown number (Pew Research Center).
Additionally, 32% of consumers say phone calls are the most frustrating customer service channel (Invoca). Given this fact, it’s no surprise that healthcare organizations are exploring other options to boost engagement.
Engage Members With Texting
Texting is a powerful communication channel with increasing adoption in the healthcare industry. Texts can help plans reach members quickly and encourage more engagement. In terms of reach, studies have shown that text messages have an astonishing average open rate of as much as 98%. That’s nearly five times more than email, which averages a 20% open rate (SMS Comparison). These numbers demonstrate the reach and impact of texting as a communication channel.

High open and read rates are not the only benefits of texting. Text messages are easily accessible on mobile devices. It’s worth noting here that Americans spend an average of 5.4 hours per day using their phones (ZDNET). This means that members not only receive the information quickly, but they can also respond at their own pace, no matter the place or time (Text-em-all).
This is a major point of difference from phone calls and emails. Calls can interrupt daily activities and emails may get lost in crowded inboxes.
The key here is that texting not only gives updates in a timely fashion, but it also makes it easy for members to take immediate action. This is one reason why texting can enhance the overall member experience and contribute to higher engagement.
We’ve explored how texting can enable health plans to improve their member outreach. Now, let’s talk about the benefits that timely updates can bring — both to members and to plans.
Benefits Of Timely Updates
Here’s a sobering statistic from McKinsey & Company: Health insurance companies’ current outreach strategies could be missing as much as 95% of potential impact.
Why are so many members choosing not to engage? It’s not because they don’t care about their health. It’s because they aren’t finding it easy and accessible to engage. Health plans that are able to innovate and provide better member communication with SMS can see significant benefits.
Benefit Utilization
Many health plans seemingly offer more and more benefits to members every year. This is fantastic for members’ health — if members actually know about the benefits and use them. Unfortunately, 35% of people don’t fully understand their healthcare coverage (HR Dive). That means that a large segment of members are probably not using all the benefits their plan provides.
By strategically sending text updates to educate members about their benefits, health plans can increase utilization. This can include reminders about preventative screenings or specialized benefits like physical therapy. Participation in these benefits can lead to higher member satisfaction and lower costs from more efficient care.

Care Management
You might not think that texting updates could play a vital role in improving health outcomes, but it can have an impact. For members in specific care management programs, SMS can help send reminders for medical appointments, lifestyle modifications, and medication adherence. This can make a big difference in health outcomes, member satisfaction, and overall cost of care.
Reducing Missed Appointments
Missed appointments are a common way that members’ healthcare gets disrupted. Texting reminders and updates about upcoming appointments can significantly reduce the number of no-shows. This ensures members receive the care they need in a timely manner. This, in turn, reduces the burden on emergency rooms, contributes to better health outcomes, and boosts member satisfaction.
Increased Member Satisfaction And Loyalty
By providing timely updates and relevant information, health plans can enhance member satisfaction and foster loyalty. Members appreciate being kept informed about changes that may affect their coverage or benefits. Regular outreach, if it’s relevant and thoughtful, shows members that their plan cares for their well-being. This increases the odds of members renewing with the plan and could even impact Medicare Star Ratings.
Go Beyond One-Way Texting With Drips
For health plans, delivering timely updates to your members is crucial for their well-being and satisfaction. Drips' Conversations as a Service is an AI-powered strategy that goes above and beyond simple text messages.
Drips reaches out to members using two-way, personalized SMS conversations. We work with large healthcare brands to effectively engage members at scale, fostering meaningful interactions and promoting active participation in their healthcare journey.
If you’re interested to learn how conversational outbound can offer best-in-class member engagement, please reach out for a demo and additional resources today.