Nine Keys To Effective Health Plan Member Onboarding
When new members enroll in a health plan, member onboarding is essential to guide them through the necessary steps to help them understand and make the most of their healthcare benefits. Onboarding goes beyond paperwork and administration — it’s an opportunity to connect with members on an emotional level, enhance their satisfaction with the plan, and empower them to take charge of their well-being.
Let’s delve into nine key tactics for achieving exceptional member onboarding. By implementing these strategies, healthcare companies can create a seamless transition for their members, fostering long-term relationships built on trust, education, and personalized support.
Why Is Onboarding Important In Healthcare?
Health is a fundamental aspect of individuals' lives and onboarding presents a unique opportunity to engage members and increase their satisfaction with their chosen health plan. Despite efforts to streamline the enrollment process, healthcare remains a complex domain, leaving many members with questions and misconceptions even after enrollment. Through onboarding outreach, health plans can educate and empower members, teaching them how to effectively utilize their benefits and begin their journey towards better health.
Keys To Best-In-Class Member Onboarding
1. The Welcome Call
The welcome call is a crucial step in making a strong first impression during health plan member onboarding. It provides an opportunity to connect with new members, set the tone for the relationship, and achieve various objectives. Expressing gratitude for choosing the plan establishes rapport, trust, and loyalty.
The value of a well-executed welcome call cannot be overstated. One simple call can reassure members of their decision and show them the expert support they will receive for their healthcare needs.
2. Assess Health Status
Health risk assessment (HRA) completion plays a vital role in a health plan's onboarding and member engagement strategy. Conducting the HRA during or shortly after the welcome call is crucial. It serves several important purposes, including capturing timely and actionable data to identify care obstacles, safety issues, and modifiable health risks before they worsen. Additionally, it helps monitor changes in health status and behaviors over time, educates members on preventive care and chronic condition management services, and provides valuable insights for critical interventions and support.
3. Establish The Patient-Physician Relationship
Establishing a strong relationship between members and primary care physicians (PCP) is vital for overall well-being as a long-term relationship with a PCP keeps people healthier (Cleveland Clinic). To simplify the daunting task of choosing a doctor, health plans can proactively assist members in selecting an in-network physician who meets their specific needs. Accurate documentation and reporting during these visits help identify members who may benefit from additional support services.

4. Provide Expert Support
Health literacy is a major challenge in the US, with only 12% of adults demonstrating proficient skills in this area (Agency for Health Research and Quality). Consequently, many members lack the knowledge to effectively use their coverage. This leads to confusion and frustration as individuals struggle to navigate the complexities of healthcare and their policies. To address this, healthcare providers should provide support like care navigation. These services help members with tasks like verifying eligibility, understanding benefits, and selecting providers — and can ultimately contribute to reduced costs and improved outcomes (EBN).
5. Strive For Seamless Interactions
In an era of increased consumer choice and responsibility in healthcare, individuals are becoming less tolerant of inconsistent interactions, inconvenient services, and a lack of personalization from their health plans. To meet these expectations, the use of advanced customer relationship management (CRM) technology is crucial. Leveraging CRM capabilities allows for seamless tracking of interactions across multiple channels, minimizing confusion caused by disjointed outreach efforts that fail to align with members' specific needs.
6. Ensure Appropriate Utilization
Promoting members' understanding of how to optimize their healthcare coverage, including distinguishing between appropriate doctor's office visits and emergency room (ER) visits, is crucial for ensuring timely and cost-effective care. Visiting the ER or urgent care centers (UCCs) for low-acuity, non-urgent conditions often result in unnecessary tests, treatments, and expenditures. Unfortunately, data indicates an upward trend in such visits (American Action Forum).
Several factors contribute to these non-emergency visits, including limited awareness of alternative care options, lack of assigned primary care physicians, and limited access to physicians. To address this issue, health plans should prioritize strategies aimed at reducing unnecessary ER and UCC utilization. This involves equipping members with the necessary tools to differentiate between urgent and non-urgent medical conditions and helping them overcome barriers to receiving appropriate care.
7. Coordinate Preventive Care
Seven out of 10 deaths among Americans each year are due to chronic diseases such as cancer, diabetes, and heart disease (Center for Disease Control and Prevention). Despite having the opportunity to prevent chronic ailments from occurring or progressing, preventive care services like mammograms, colonoscopies, and vaccinations by Americans are significantly underutilized (Center for Disease Control and Prevention). To improve preventive care utilization, it’s important to not only understand and address the myriad barriers people face, but also to assist them with coordinating their care.

8. Anticipate Common Issues
Understanding and addressing common issues is a fundamental part of providing exceptional member onboarding in healthcare. By anticipating frequently asked questions and potential challenges, health plans can proactively educate their members and enhance their overall experience.
Take, for instance, a health plan that emphasizes virtual care services. Recognizing that some members may be unfamiliar with this approach, the plan can take proactive steps to educate new enrollees. They can offer clear instructions on how to schedule virtual appointments, highlight the advantages and convenience of virtual care, and address any doubts or misconceptions that members might have.
9. Highlight Popular Benefits
Highlighting popular benefits is a crucial element of effective health plan member onboarding. Healthcare is very complex and many members may only have a basic understanding of the plan features when they enroll. Therefore, during the onboarding process, it’s essential to emphasize and educate members about the popular benefits of their plan. This can be done through targeted communication, such as personalized messages, and interactive tools that showcase the value and advantages of specific benefits.
Let's consider a health plan that offers a comprehensive wellness program as a benefit. Instead of assuming that members are aware of the program's advantages, the plan can send personalized messages highlighting success stories of individuals who have used the program to achieve positive health outcomes. By showcasing the tangible benefits and emphasizing the potential impact on the member's well-being, the health plan effectively sells the member on the value of the wellness program. Without this outreach, the member may have never explored this benefit.

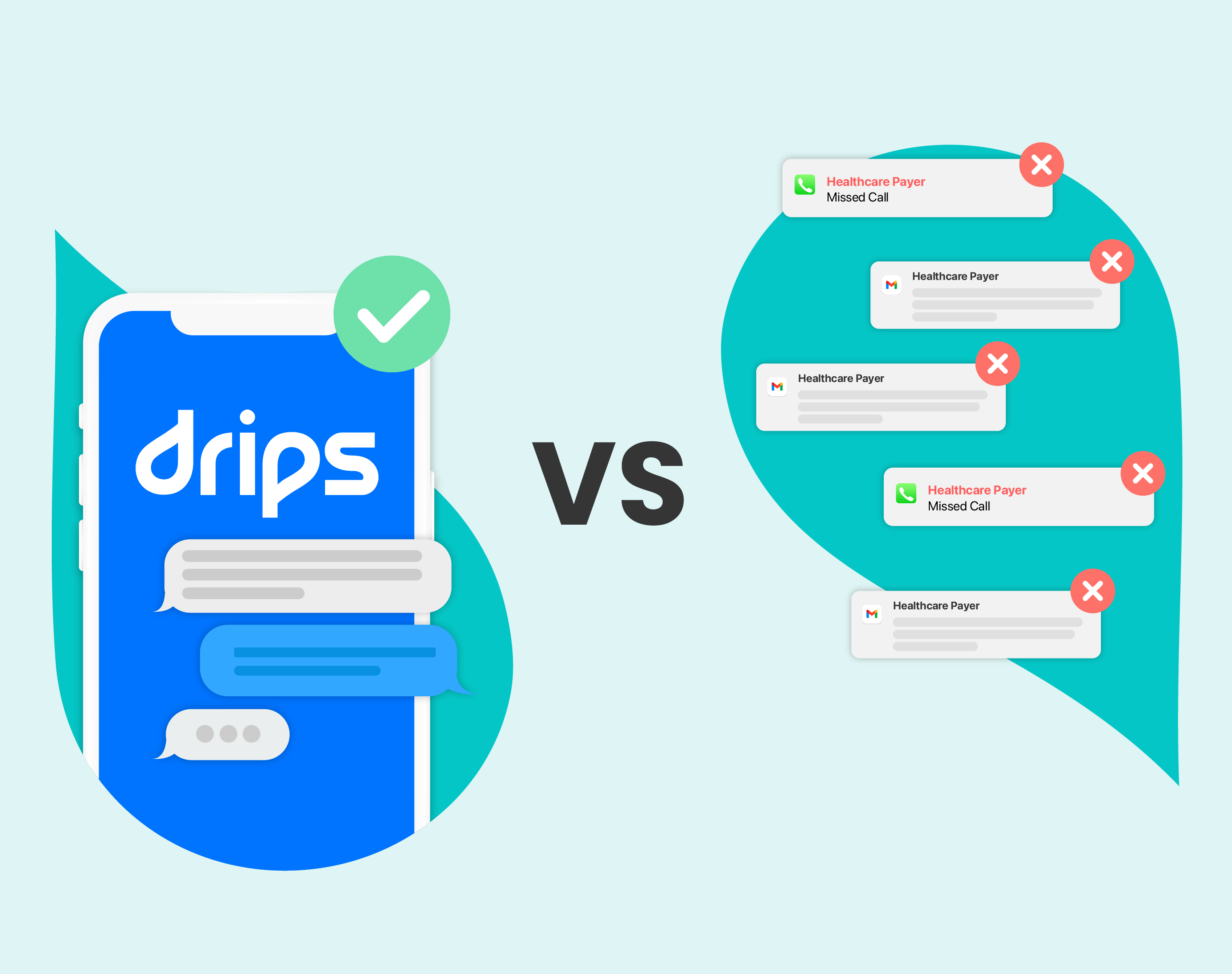
Drips Is A Proven Onboarding Solution
Drips' conversational outbound strategy is a proven solution for member onboarding that offers a brand new strategy for encouraging new members to engage on their own terms for better overall results. Using empathetic messaging powered by conversational AI, Drips helps plans provide personalized onboarding experiences. This innovative approach allows health plans to deliver relevant information, answer questions, and address concerns in real time, fostering a sense of trust and connection from the very beginning.
This engagement meant that these members were getting a better experience and more information about their health plan.
Want to hear the whole story? Read the case study now.