How To Optimize Health Plan Member Outcomes
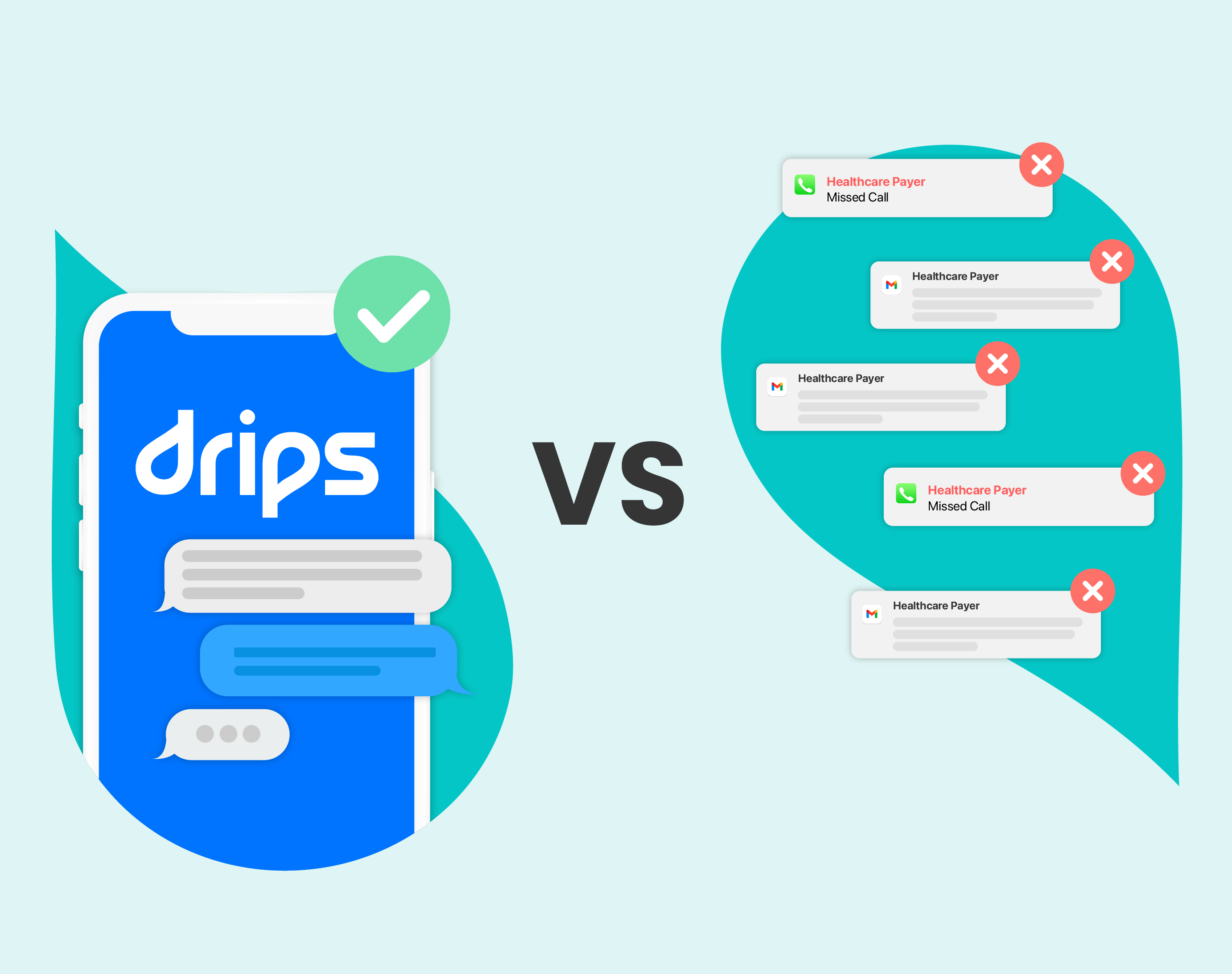
Today’s onslaught of unwanted calls and emails has made it incredibly difficult for health insurance providers to connect with members who have a lot of unmet medical needs. To change this behavior in high-risk populations, healthcare professionals must now consider better ways to communicate with their members because simply contacting people isn’t good enough anymore.
The desire for payors to improve health outcome performance has never been more urgent. What’s prompting this change and why is the quality of engagement the answer? Let’s take a look
What’s Driving The Need For Engagement?

One of the biggest drivers for member engagement (which also has major financial implications for insurers) is the change the Centers for Medicare & Medicaid Services (CMS) made to the Medicare Advantage Star Rating scores this year. This change doubled the original 2X Medicare Consumer Assessment of Healthcare Providers and Systems (CAHPS) measurement to 4X, meaning that 32% of the star rating will now be based on patient experience (PSQH), making it more important than ever for members to take full advantage of their benefits.
As you probably know, a higher star rating comes with some pretty great benefits. Plans rated three-and-a-half stars or less are paid a base rate based on the county in which it enrolls beneficiaries. However, if the plan increases the rating to four stars or more, it is paid a 5% bonus in addition to the base rate.
The most significant incentive is reserved for healthcare plans with a five-star rating, which can enroll members throughout the year, not just during the fall annual election period. And on top of that, plans receiving a bonus payment also get a better rebate level.
Because of the financial benefits, the need to improve a patient’s experience is too high to ignore. And what’s the best way to do that? Driving high-quality engagement.
Improving The Member Experience & Driving Outcomes

If you want to drive member engagement and optimize outcomes within value-based healthcare models, you’ll need to improve the quality of care for members identified as “complex,” or within a high-risk population group. Generally, that’s achieved by focusing on three areas:
- Early intervention for preventing a decline in quality of life and cost to fight disease.
- Behavioral health to implement lifestyle changes designed to halt disease progression.
- Educating members on best practices regarding annual wellness visits, preventive care, and health plan benefit utilization (RISE).
Most healthcare insurance providers rely on call centers to communicate with their members, but there's a massive challenge with the most popular outreach strategy — people don’t pick up the phone if they don’t know the number (or if they’re busy). So, if health insurers want to achieve a high star rating, they’ll need to reinvent how they engage with their members.
Adding an AI-powered conversational outreach platform will drive more personalized conversations and increase high-intent inbound call traffic. Rather than relying on one-way outreach methods, a conversational outreach approach encourages engagement on multiple fronts. It also puts the power in the audience’s hands while still being persistent.
Benefits Of A Conversational Outbound Approach

Drips Conversations as a Service combines AI-powered two-way texting, proactive calls, and voicemail messages designed to improve patient engagement. This allows you to put the member in charge of the conversation, enabling them to connect with you on their terms. The result?
- Increased number of inbound engagements
- Prepared members expecting scheduled calls
- Improved quality of interaction
- More members taking control of their health
Simply put — you can’t improve a member’s health outcome without productive member engagement. And to do that, you need a modern outreach approach that leverages AI technology.
Want to work towards improving or maintaining your star rating?